20 MHz高频超声在瘢痕评估中的应用
本文来源:《中华整形外科杂志》2023年6月 第39卷 第6期
DOI:10. 3760 / cma.j.cn114453-20220320-00075
作者单位:空军军医大学第一附属医院烧伤与皮肤外科, 西安710032
通信作者:李娜,Email:linaxjss@163.com
【摘要】
目的 探讨20 MHz高频超声在瘢痕厚度及形态学评估中的作用。
方法 对2019年4月至2020年12月空军军医大学第一附属医院烧伤与皮肤外科诊治的烧创伤后瘢痕形成初期(<1个月)、增生期(1~6个月)和消退期(>6个月)患者的临床资料进行回顾性分析。全部纳入患者均进行了20 MHz高频超声、温哥华瘢痕量表(VSS)及病理组织学3种方式的评估。超声检查时在瘢痕处选择3个点进行瘢痕厚度测量,记录平均值;在超声测量部位的瘢痕组织取标本,进行HE染色和Masson染色,观察并测量瘢痕厚度;由2名医生采用VSS对瘢痕的厚度进行评估,记录平均值。分别比较瘢痕形成初期、增生期、消退期采用上述3种方式测评的瘢痕厚度的差异;同时,对比高频超声声像图特征与病理组织形态学的关系。正态分布计量资料以±s表示,3组间比较采用单因素方差分析,组间两两比较采用SNK-q检验;计数资料采用卡方检验进行分析。
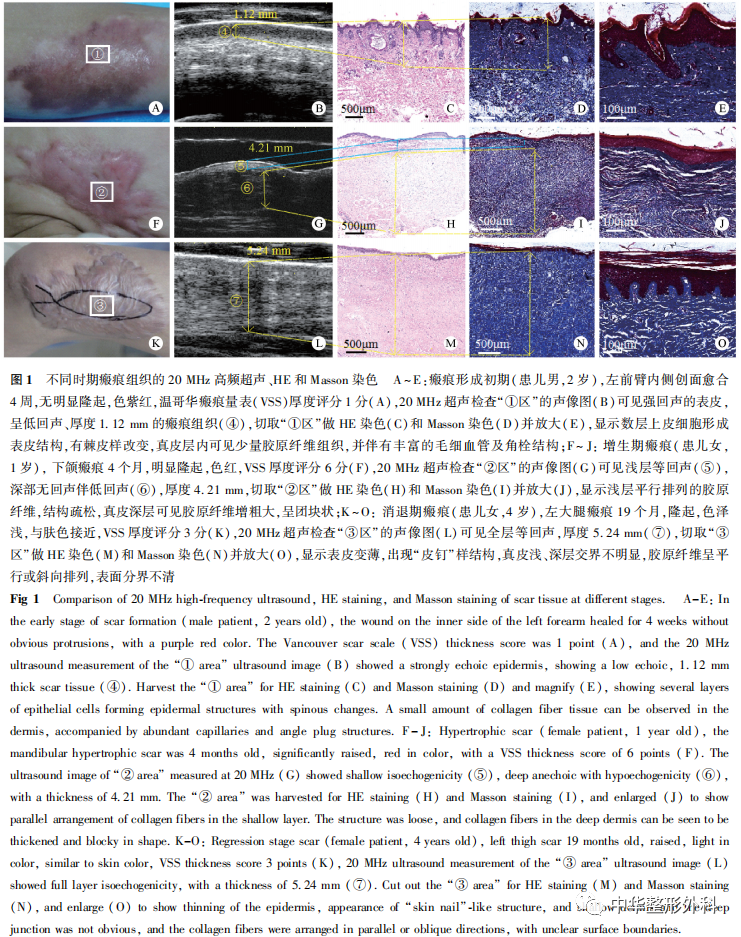
结果 共纳入224例患者,男91例, 女133例,年龄1~34岁,平均25.7岁;瘢痕形成初期患者79例、增生期102例、 消退期43例。(1)在瘢痕形成初期,20 MHz超声测量的瘢痕厚度为(2.01±0.68)mm,VSS评估厚度为(1.72±0.49)mm,病理测量厚度为(2.11±0.45)mm;在增生期瘢痕,20 MHz超声测量厚度为(4.11±0.73)mm,VSS评估厚度为(3.02±0.47)mm,病理测量厚度为(4.27±0.44)mm;在消退期瘢痕,20 MHz超声测量厚度为(1.74±0.64)mm,VSS评估厚度为(1.77±0.61)mm,病理测量厚度为(1.71±0.67)mm。对于3个时期的瘢痕,20 MHz高频超声测量的瘢痕厚度与病理测量厚度的差异均无统计学意义(P均>0.05);而在瘢痕形成初期及增生期,VSS评估的厚度值与20 MHz高频超声、病理测量厚度的差异均有统计学意义(P均<0.05)。(2)在瘢痕形成初期,高频超声显示表皮厚度与正常表皮接近且呈高亮强回声,但表皮与真皮层之间有约<1 mm厚的条形低回声或无回声区,形似真皮水肿;病理组织学显示,该期瘢痕的表皮有棘皮样改变,真皮层内有丰富的毛细血管,并有少量胶原纤维组织。在增生期瘢痕,表皮仍呈强回声,真皮层内呈不均匀回声,真皮浅层呈明显等回声,而深层表现无回声或低回声;病理显示,表皮薄而光滑,角化明显,真皮浅层可见与表面平行、排列规则的胶原纤维,真皮深层可见胶原纤维增多增厚,呈结节状、漩涡状。在消退期瘢痕,表皮呈强回声,真皮层与皮下组织之间无明显分界,呈均匀等回声;病理显示,表皮变薄,出现“皮钉”样结构,真皮浅、深层交界不明显,胶原纤维呈平行或斜向排列,表面分界不清。
结论 20 MHz高频超声对瘢痕厚度的评估较VSS更准确,且可反映瘢痕内胶原分布、水分比例情况,相较于病理检查具有无创、快捷的优点,是评估瘢痕厚度及形态学的有效手段。
【关键词】瘢痕;超声检查;高频超声;病理学;Masson染色;温哥华瘢痕量表;瘢痕厚度
Application of 20 MHz high-frequency ultrasound in scar evaluation
Bai Lu, Shi Xueqin, Yang Li, Zhao Wenli, Li Na, Han Juntao, Hu Dahai
Department of Burn and Cutaneous Surgery, the First Affiliated Hospital of Air Force Medical University, Xi’an 710032, China
Corresponding author: Li Na, Email: linaxjss@163.com
【Abstract】
Objective To investigate the role of 20 MHz high-frequency ultrasound in evaluating scar thickness and morphology.
Methods The clinical data of patients with the initial stage of scar formation after burn trauma (<1 month), hypertrophic scar (1-6 months) and atrophic scar (>6 months) treated by the Department of Burn and Cutaneous Surgery, the First Affiliated Hospital of Air Force Medical University from April 2019 to December 2020, were retrospectively analyzed. All patients were evaluated by 20 MHz high-frequency ultrasound, histopathology and Vancouver scar scale (VSS). Three measurement points were randomly selected at the scar during ultrasonic examination, and the average value was recorded as the ultrasonic thickness measurement value. The scar tissue samples were collected from the site of ultrasonic examination, and HE staining and Masson staining were performed. At the same time,scar thickness was evaluated by two physicians using VSS. The difference of scar thickness assessment result among the 3 method in patients at the initial stage of scar formation, hypertrophic scar and atrophic scar was compared. Meanwhile, the relationship between the characteristics of 20MHz high-frequency ultrasound and histopathology was compared. The measurement data of normal distribution were expressed as Mean±SD. One-way ANOVA was used for comparison among three groups, and SNK-q test was used for pairwise comparison between groups. Counting data were analyzed by Chi-square test.
Results A total of 224 patients were included, including 91 males and 133 females, aged from 1 to 34 years, with an average age of 25.7 years. There were 79 patients at the initial stage of scar formation, 102 at the hypertrophic stage, and 43 at the atrophic stage. (1) In the initial stage of scar formation, the thickness measured by 20 MHz ultrasound was about (2.01±0.68) mm, the thickness evaluated by VSS was (1.72±0.49) mm, and the thickness measured by pathological section was (2.11±0.45) mm. In the hyperplastic scar stage, the thickness measured by 20 MHz ultrasound was (4.11±0.73) mm, the thickness evaluated by VSS was (3.02±0.47) mm, and the thickness measured by pathological section was (4.27±0.44) mm. In the atrophic scar stage, the thickness measured by 20 MHz ultrasound was (1.74±0.64) mm, the thickness measured by VSS was (1.77±0.61) mm, and the thickness measured by pathological section was (1.71±0.67) mm. For scars in the above three periods, there was no statistical significance between scar thickness measured by 20 MHz high-frequency ultrasound and that measured by pathological sections(all P<0.05). In the initial stage of scar formation and hypertrophic stage, the thickness evaluated by VSS was significantly different from that measured by 20 MHz high-frequency ultrasound and pathology (all P<0.05), respectively. (2) Echo intensity was evaluated by ultrasound. In the initial stage of scar formation, the thickness of the epidermis shown by high-frequency ultrasound was close to that of the normal epidermis and presented a high-intensity echo, but there was a strip of echoless or no echo zone of <1mm between the high-intensity echo epidermis and dermis, which looked like dermal edema. Pathology showed that there were acanthoid changes in the epidermis of the scar at this stage, rich capillaries and a small amount of collagen fibrous tissue in the dermis. In the hyperplastic scar stage, the scar epidermis still showed strong echo, while the dermis showed uneven echo, the superficial dermis showed obvious isoecho, and the deep dermis showed no echo or hypoecho. Pathology showed that the epidermis was thin and smooth, and keratosis was obvious. Collagen fibers parallel to the epidermis could be seen in the superficial layer of the dermis, with regular arrangement. Collagen fibers were increased and thickened in the deep layer of the dermis, in the shape of nodules and swirls. In the atrophic scar stage, the scar epidermis presented a strong echo, and there was no obvious demarcation between the dermis and subcutaneous tissue, presenting a uniform echo. Pathological findings showed that the epidermis became thinner with a “skin nails”-like structure, the junction between the superficial and deep dermis was not obvious, and the collagen fibers were arranged in parallel or oblique direction, and the surface boundary was unclear.
Conclusion 20MHz high-frequency ultrasound is more accurate than VSS in the assessment of thickness of hypertrophic scar, and can reflect the collagen content and moisture ratio in scar. Compared with pathological examination, it has the advantages of non-invasive and fast, and is an effective means to evaluate scar thickness and morphology.
【Key words】Cicatrix; Ultrasonography; High-frequency ultrasound; Pathology; Masson staining; Vancouver scar scale; Scar thickness
Disclosure of Conflicts of Interest: The authors have no financial interest to declare in relation to the content of this article.
Ethical Approval: This study was conducted in accordance with the Helsinki Declaration.
瘢痕是烧创伤后组织修复的必然结果。近年来瘢痕防治越来越受到关注,治疗方法也逐渐增多。在常规的硅酮药物、压力治疗的基础上,激光疗法、肉毒毒素或糖皮质激素局部注射等也获得了该领域专家的认可,并写入瘢痕治疗的指南中[1-2]。但个体差异、医生的治疗经验、治疗方案的选择等会导致瘢痕治疗效果参差不齐。准确、有效的瘢痕评估是治疗方案选择、技术参数改进、瘢痕量化管理不可或缺的重要组成部分,因此提高瘢痕评估的准确度显得尤为重要。温哥华瘢痕量表(Vancouver scar scale, VSS)是瘢痕评估简单、快捷且常用的方法[3],但对于瘢痕增生初期的水肿、未突出体表的皮下瘢痕,其厚度不易判断,很难准确评估;且在瘢痕的质地评分上,“柔软”与“柔顺”的区别也很难把握。B型超声是评估组织厚度、组织结构最常用且准确快捷的方法。高频皮肤超声因兼顾探测深度、表皮-真皮界限而广泛用于临床皮肤检测[4]。瘢痕组织主要分布在近似真皮层及浅筋膜层,20MHz高频超声是观察表皮、真皮及浅筋膜层皮损的最佳监测设备[5-6]。本研究通过对烧创伤后瘢痕形成初期、增生期和消退期患者的20MHz高频超声、病理组织学、VSS评估情况进行分析比较,探讨20MHz高频超声作为瘢痕常规评估工具的可行性。
资料与方法
一、 资料选择
收集2019年4月至2020年12月空军军医大学第一附属医院烧伤与皮肤外科诊治的烧创伤后瘢痕形成初期(<1个月)、增生期(1~6个月)和消退期(>6个月)患者的临床资料,进行回顾性分析。纳入标准:瘢痕形成初期、增生期、消退期患者,无明显瘢痕挛缩畸形及功能障碍。排除标准:近3个月使用糖皮质激素类药物;测量部位伴有病毒或细菌感染;怀孕或哺乳;不能按期随访。
患者或家属对研究知情,并同意将资料用于本研究。本研究已参考赫尔辛基宣言。
二、 方法
分别比较瘢痕形成初期、增生期、消退期患者采用20MHz高频超声、病理组织学及VSS 3种方式评估的瘢痕厚度的差异;同时,对比20MHz高频超声声像图特征与病理组织形态学的关系。
(一)20MHz高频超声
所有患者瘢痕部位检测前与患者进行沟通,介绍超声评估的目的,检测前清洁瘢痕皮肤,使用单反数码相机(佳能EOS 650D型)拍照并存档。所有病变均采用高频超声皮肤诊断系统(天津迈达医学科技股份有限公司,型号MD-3000S)进行检查。如果瘢痕是不规则的,以瘢痕最厚区域代表该部位瘢痕的厚度,检查中用20 MHz线性探头选择3个测量点,测量瘢痕厚度和回声强度,记录厚度平均值。通过与周围正常组织的比较来评估瘢痕的回声强度,分为4种:高回声、等回声、低回声及混合回声。
(二)VSS评估
所有瘢痕由2名医生采用VSS进行评分,以平均值作为该瘢痕的评分值。主要从色泽、厚度、血管分布、柔软度4个指标对瘢痕进行评估,量表总分为15分,评分越高表示瘢痕越严重。色泽:0分为正常颜色,1分为浅白色或浅粉红色,2分为深浅混集,3分为深色;厚度:0分为正常,1分为>0~1 mm,2分为>1~2 mm,3分为>2~4 mm,4分为>4 mm;血管分布:0分为正常,1分为粉红色,2分为红色,3分为紫色;柔软度:0分为正常,1分为柔软,2分为少许拉紧,3分为质硬,4分为牵拉关节弯曲、关节很难伸直,5分为形成永久性软组织挛缩如关节畸形。
(三)瘢痕组织病理染色
在超声测量部位的3个点中选择最接近平均值的点,切除瘢痕组织取标本。获取瘢痕组织后纵行剖开,以4%多聚甲醛固定并编号,石蜡包埋,厚度为5 μm进行连续切片,然后进行脱蜡、透明、HE及Masson染色,光镜下观察并测量瘢痕厚度。
三、统计学处理
采用SPSS 18.0统计软件进行数据分析。患者年龄、瘢痕厚度为正态分布计量资料,以±s表示,3组间比较采用单因素方差分析,采用SNK-q检验进行组间两两比较;患者性别构成比、皮肤类型构成比为计数资料,以例(%)表示,采用卡方检验进行分析。以P<0.05为差异有统计学意义。
结 果
一、一般资料
......